Cartilage Resections
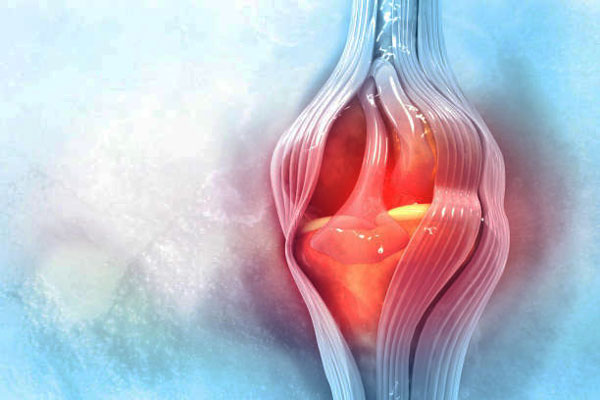
Cartilage is the white tissue that lines and protects the ends of bones and helps these bones connect and form joints. It acts as a shock absorber and also helps in the smooth gliding of bones during their movement. Cartilage is usually damaged due to trauma and wear and tear with increasing age. This can lead to pain and, at times, swelling, making it difficult to maintain an active lifestyle. Cartilage damage is common in the knee but is also found in the ankle, hip, and elbow.
With the advancement of technologies, it is possible to repair cartilage damage that is limited to a specific area with cartilage restoration treatments.
What is cartilage restoration?
Cartilage restoration treatment is a compilation of various surgical treatments to repair cartilage damage limited to one area. However, cartilage restoration techniques are not applicable to treat damages that are present throughout a joint or those from osteoarthritis or other forms of arthritis because the articular cartilage (present at the ends of the bones) fails to regrow or heal in such conditions. Cartilage restoration is an early treatment option that can delay or prevent the need for joint replacement surgery.
The surgery is done arthroscopically or by a formal open procedure where the orthopedic surgeon stimulates the growth of new cartilage tissue that can restore the normal functions of the damaged cartilage. Common techniques used to stimulate the growth of new cartilage include microfracture, drilling, and abrasion arthroplasty.
Indications for cartilage restoration surgery
Cartilage restoration is recommended for people who are young and have minor cartilage injuries that are relatively recent and limited in the area involved, as well as for those who have prolonged joint pain not because of arthritis.
The treatment is applicable for patients with knee cartilage damage or deterioration caused by:
- Injury or trauma
- Repetitive injuries
- Congenital abnormalities (by birth) affecting the normal joint structure
- Hormonal disorders that affect the development of bones and joints, such as osteochondritis dissecans (OCD).
What is the pre-procedure care?
Many procedures are available to restore cartilage. Before finalizing the cartilage repair approach that is best for you, a magnetic resonance imaging (MRI) test is performed to determine the severity, size, and location of cartilage injuries.
Once your surgeon finalizes the approach for cartilage restoration surgery, you will be prepared for the surgery by taking the following measures:
- A complete physical examination, blood tests, imaging tests, etc. will be performed to ensure that you don't have any conditions that could interfere with the surgery or its outcome.
- You may be asked to temporarily discontinue certain medications prior to surgery as they may increase the risk of bleeding or other complications during the procedure.
- If you are overweight, you may be advised to lose weight before surgery to reduce pressure on your newly restored joint.
- You should stop smoking to reduce surgery risks and improve recovery.
- You must carry loose-fitting clothes that are comfortable while moving around, resting, and for physiotherapy.
- You will be asked not to eat or drink 6-8 hours before the surgery, as food and anesthesia can often cause nausea or vomiting.
- The anesthesia team, along with the surgeon, will meet you prior to the surgery to assess your health and ensure that your anesthesia care is as safe and effective as possible.
How is cartilage restoration performed?
The cartilage restoration treatment aims to restore cartilage either by stimulating the growth of new, healthy cartilage or repairing it with healthy transplants. Most procedures are carried out arthroscopically, and in some cases, open surgeries are required, which require longer and more open incisions to get direct access to the affected area.
In arthroscopic surgeries, the surgeon will make three small incisions around the injured joint and will insert an arthroscope (a thin tube with a tiny camera) through one of these incisions. This camera will give a clear internal view of the joint, which helps the surgeon visualize, diagnose, and treat the condition.
The common procedures for cartilage restoration are:
- Arthroscopic microfracture: It is an arthroscopic procedure that aims to stimulate the growth of new cartilage by creating a new blood supply. Holes are made in the bone beneath the damaged cartilage (subchondral bone), which lets the area bleed. This action triggers the healing response, as the blood supply will bring cells that can stimulate cartilage growth and the formation of fibrocartilage in the injured area.
- Arthroscopic debridement: In arthroscopic debridement, the torn or damaged cartilage is located using the arthroscope and trimmed away using sharp surgical tools like scalpels, curettes, forceps, or scissors.
- Abrasion arthroplasty: This procedure will stimulate the potential cells that can form new cartilage tissues within the defective area. High-speed burrs are used to remove the defective cartilage and penetrate to reach the subchondral bone. This will trigger the blood cells to create a healing response.
- Articulated cartilage implantation (ACI): It is a procedure where new cartilage cells are grown and implanted in the defective cartilage. The total procedure involves two steps. The first step is to collect healthy cartilage tissue from the patient's body. The tissue is then processed in a laboratory to produce chondrocytes (cells that produce cartilage). The second step is to re-implant these chondrocytes in the area where there's been cartilage loss.
Though the procedure is highly successful in treating cartilage damage, it has the drawback of requiring a longer recovery time as it requires an open incision. - Osteochondral graft transfer: In this procedure, healthy cartilage tissue (a graft) is collected and transferred to the defective joint. The graft can be either autograft (taken from the patient's body) or allograft (taken from a cadaver or donor). Autograft transplant is applicable for patients with smaller cartilage defects, while allograft is used in cases with a large cartilage defect (greater than two centimeters in diameter). The procedure is performed through an open incision where the graft is contoured to the exact shape of the defect and then fitted into place.
What is the post-procedure care?
After the surgery, it is important to take care of the joint surfaces until the cartilage heals. You will be on crutches for six to eight weeks to avoid putting pressure on the affected area.
Physical therapy is vital for proper recovery. Your surgeon will refer you to a physiotherapist, who will recommend some exercises that will help restore mobility to the affected joint.
You will be advised to keep the area in an elevated position to avoid swelling and inflammation. You will have frequent follow-up visits where the surgeon will assess your recovery. Your surgeon will monitor how well your new cartilage is developing and merging with existing cartilage.
The recovery time varies with the surgical technique you have undergone. Usually, it takes a minimum of 2-3 months to return to your normal activities.
Outlook
Cartilage restoration is the treatment option for young adults with a minor cartilage injury or lesion. As a healing process, the therapy focuses on repairing or regrowing the affected cartilage. The major advantage of cartilage restoration treatments is that they can be tailored according to the patient's needs. As most of the procedures are performed arthroscopically, the recovery is quick and less painful.
The rehabilitation procedure will focus on strengthening the joint and the muscles that support it. It may take a few months for the patient to return to their normal activities.
